RPE-based training – What is the Borg RPE Scale and how can I apply it to my workouts?
What is RPE?
The Borg Rating of Perceived Exertion (RPE) Scale is a subjective scale which is used to estimate one’s own level of exhaustion. The original scale was a 6-20 scale, relating to heart rate, whereby 6 denotes a resting intensity and 20 is maximal intensity. For simplicity, there exists a modified scale of 1-10.
RPE can be applied to both resistance exercise and cardiovascular exercise and is usually obtained either immediately following a bout of exercise or after the session is complete (session-RPE). The Borg Scale defines an exercise to be of a particular intensity based on the range it sits in (see figure below for details). The RPE scale offers an intuitive approach to exercise in the form of self-monitored training intensity.
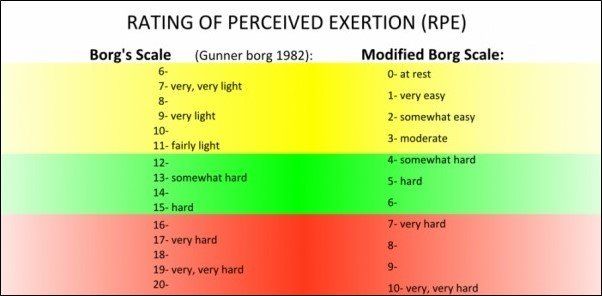
It should be noted that despite distinct categories of light, moderate and hard intensity, the RPE scale is more accurately represented as a spectrum.
Given time and practice, the Borg RPE Scale can yield more accuracy and consistency as one’s perception of exertion will improve. Coaches may also ask for a client’s RPE to gauge their progress and difficulty of the session.
How can I apply RPE to my own training?
RPE can be set at a pre-determined value prior to performing a set or bout of exercise. On days when energy levels are diminished, or when working through an injury, deliberately working at a low RPE could be a viable strategy to avoid excessive fatigue and prevent further injury. An example of this would be acquiring a knee injury and decreasing the amount of weight lifted on squats, effectively lowering the RPE.
On the other hand, on days where energy levels are high and performance seems to be at its peak, training at a high RPE could be beneficial. For instance, testing 1-repetition-max performance requires RPE 10, therefore it would be more appropriate to perform this on days with higher energy levels to avoid injury.
This method of adjusting the session intensity as you go is a sustainable way to approach training and may be appropriate for the majority of people. It is important to keep in mind that for people with specific training goals and deadlines such as competitions, abiding by the programmed intensity leading up to competition could yield a better outcome.
If strength progression is a goal, an individual may notice that their RPE for a given set performed each week may be slowly dropping, implying that strength has increased and therefore it would be time to increase the weight. This method of tracking progression may also apply to other forms of exercise such as running. Performing a 5km run may invoke a post-session RPE of 9, but after completing the same run frequently for 2 months at the same pace, the RPE may drop to 7, indicating that it is time to increase the pace or distance.
How hard should I be working?
RPE should be varied across a training program such that each week is not consistently at a high RPE in order to avoid burnout and fatigue. It is impossible to sustain a session-RPE of 9-10 for every session. With this in mind, the optimal RPE range to work within would be 6-10. This recommendation varies slightly throughout the current literature and there also exists newer studies which investigate low RPE coupled with high frequency training for hypertrophy. However, for the most part, training at a reasonably high RPE will return good results and let one feel accomplished after the workout.
RPE vs RIR
RPE is often used synonymously with Repetitions in Reserve (RIR), another method of subjectively scoring intensity. RIR describes the number of repetitions which could have been performed at the end of a given set, ie. The number of repetitions that were “left in the tank”. For example, after completing a set of 5 repetitions on the deadlift, one may think they could have done 2 more repetitions if they really tried. In this case the RIR would be 2, and their RPE could be somewhere between 7-9 depending on how they felt after the set. There is a slight discrepancy between these two subjective measures, however both will help gauge a similar finding.
The Borg RPE Scale is extremely useful for day-to-day exercise sessions. It can be used to track exercise progression and to adjust exercise intensity accordingly. It also encourages workouts to be completed at lower energy/effort levels on days where we simply aren’t feeling it, reminding us that doing something is definitely better than doing nothing.
References
[Image]: USING THE RPE SCALE - CMS Fitness Courses https://cmsfitnesscourses.scdn6.secure.raxcdn.com/wp-content/uploads/2018/12/cms-fitness-courses-rpe.jpg
Ciolac, E. G., Mantuani, S. S., Neiva, C. M., Verardi, C. E. L., Pessoa-Filho, D. M., & Pimenta, L. (2015). Rating of perceived exertion as a tool for prescribing and self regulating interval training: a pilot study. Biology of Sport, 32(2), 103-108.
https://doi.org/10.5604/20831862.1134312
Haddad, M., Stylianides, G., Djaoui, L., Dellal, A., & Chamari, K. (2017). Session-RPE Method for Training Load Monitoring: Validity, Ecological Usefulness, and Influencing Factors. Frontiers in Neuroscience, 11(612), 1-14.
https://doi.org/10.3389/fnins.2017.00612
Loomis, B. (2021). Struggling with RPE? This is the blog for you. 3D Muscle Journey. https://3dmusclejourney.com/struggling-with-rpe/