Shrugging Off Your Shoulder Pain?
Many people have unfortunately had to suffer a shoulder injury in some form at some point in their lives and it’s common to fall into the belief that there’s nothing that can be done except to tolerate the symptoms associated with it. These symptoms vary significantly and include a combination of things like lack of sleep, pain and even discontinued day-to-day use of the affected limb due to a lack of confidence and fear of increased symptoms. Adding to that, it often gets worse the longer it is left untreated, but the good news is that there is more available evidence out there that highlights the benefits of treating conservatively.
As Exercise Physiologists working in the Worker’s Compensation system, we see a lot of shoulder injuries and prescribe specific exercises to treat various shoulder pathologies that have either happened due to a freak accident or are the result of gradual degeneration caused by repetitive movements required by the demands of a physical job role.
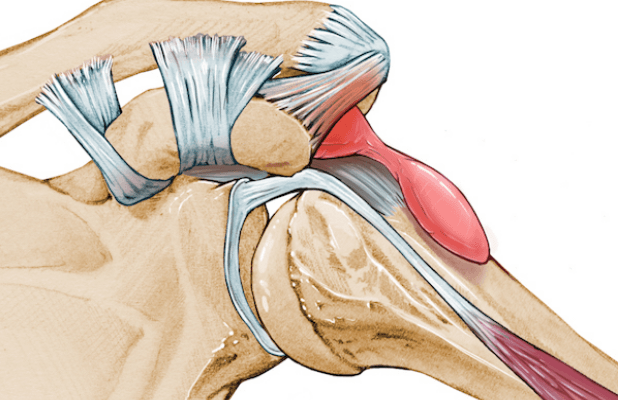
Shoulder impingement is a common issue that we see and often affects people who are doing a lot of overhead-type movements that are above 90 degrees. The pathology can be described as a condition where the subacromial structures between the humeral head and coracoacromial arch are compressed, causing various signs and symptoms. Commonly, these symptoms may include restricted range of motion, decreased strength of the upper-limb and increased reported pain. Both Clausen et al and Sharma et al., agree that there is a major reduction in strength found in people affected by shoulder impingement, particularly with shoulder external rotation and abduction movements, which may be caused by muscular conditioning following the onset of shoulder impingement as well as deficits in motor control of the muscles.
Fukunaga et al., discussed eccentric-focused exercise was found to be effective for shoulder rehabilitation by activating the rotator cuff muscles, which put simply, are a group of muscles responsible for keeping the ball of our humerus (upper arm bone) in the shoulder socket and giving us the ability to move our arms over our heads, swim, play sports like tennis and volleyball e.t.c due to the unique anatomical make-up that allows the shoulder to move in a multitude of directions. Shoulder impingement may also be associated with muscular imbalance; therefore; careful examination of flexibility and strength of important muscles about the shoulder complex is vital to understanding the root cause of impingement and prescribing effective treatment. By understanding muscular imbalances associated with impingement, physical therapists can prescribe appropriate exercises for both treatment and prevention (Page P).
If you or someone you know is currently suffering from a shoulder injury, please feel free to get in touch with us today for one-on-one support and assistance with effective return to work and improved quality of life.
Chris Chen (BSc – Exercise Physiology)
Senior Accredited Exercise Physiologist
Satpute K, Reid S, Mitchell T, Mackay G, Hall T. Efficacy of mobilization with movement (MWM) for shoulder conditions: a systematic review and meta-analysis. J Man Manip Ther. 2021 Aug 1:1-20. doi: 10.1080/10669817.2021.1955181. Epub ahead of print. PMID: 34334099.
Fukunaga T, Orishimo KF, McHugh MP. Electromyographic analysis of select eccentric-focused rotator cuff exercises. Physiother Theory Pract. 2021 Jul 27:1-9. doi: 10.1080/09593985.2021.1949767. Epub ahead of print. PMID: 34313183.
Sharma S, Ghrouz AK, Hussain ME, Sharma S, Aldabbas M, Ansari S. Progressive Resistance Exercises plus Manual Therapy Is Effective in Improving Isometric Strength in Overhead Athletes with Shoulder Impingement Syndrome: A Randomized Controlled Trial. Biomed Res Int. 2021 Jun 30;2021:9945775. doi: 10.1155/2021/9945775. PMID: 34307681; PMCID: PMC8266437.
Clausen MB, Bandholm T, Rathleff MS, Christensen KB, Zebis MK, Graven-Nielsen T, Hölmich P, Thorborg K. The Strengthening Exercises in Shoulder Impingement trial (The SExSI-trial) investigating the effectiveness of a simple add-on shoulder strengthening exercise programme in patients with long-lasting subacromial impingement syndrome: Study protocol for a pragmatic, assessor blinded, parallel-group, randomised, controlled trial. Trials. 2018 Mar 2;19(1):154. doi: 10.1186/s13063-018-2509-7. PMID: 29499710; PMCID: PMC5833202.
Page P. Shoulder muscle imbalance and subacromial impingement syndrome in overhead athletes. Int J Sports Phys Ther. 2011 Mar;6(1):51-8. PMID: 21655457; PMCID: PMC3105366